Artificial intelligence is rapidly reshaping the healthcare industry, and medical coding is one of the areas receiving the most attention. With AI-powered medical coding software now capable of scanning clinical notes and suggesting CPT, ICD-10, and HCPCS codes, many healthcare professionals are asking an important question: will AI replace medical coders?
The concern is understandable. Automation has already changed billing workflows, claims submission, and eligibility verification. However, the reality is far more nuanced. While AI is becoming an important part of medical billing and coding, it is not positioned to fully replace certified medical coders. Instead, AI is redefining how coding work is performed and where human expertise remains critical.
Why AI Is Being Adopted in Medical Coding
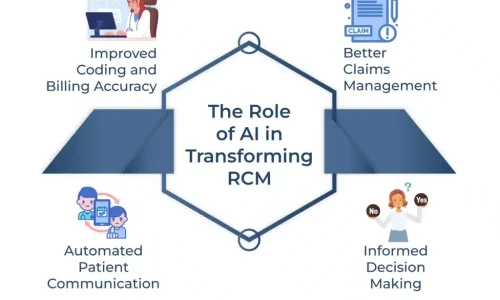
Medical coding is a time-consuming and detail-heavy process. AI-driven coding tools are designed to reduce manual effort by analyzing electronic health records and extracting relevant data points. These systems can quickly identify diagnoses, procedures, and modifiers, allowing practices to process claims faster and reduce backlogs.
From a revenue cycle management perspective, this speed is attractive. Faster coding often means faster claims submission and potentially improved cash flow. For high-volume practices, AI-assisted medical coding can help manage workload during peak periods.
However, speed alone does not guarantee accuracy or compliance, which are the most important factors in medical billing.
What AI Can Do Well in Medical Coding
AI performs best when encounters are straightforward and documentation is clean. For routine office visits, common diagnoses, and standardized procedures, AI can accurately suggest codes and reduce repetitive tasks for coding teams.
AI also excels at pattern recognition. It can flag missing documentation, identify inconsistencies, and highlight potential coding gaps. When used correctly, this helps medical coders focus more on quality control rather than manual data entry.
In short, AI is effective as a support tool within the medical coding workflow.
Where AI Falls Short and Why Human Coders Are Still Essential
Despite its strengths, AI lacks clinical judgment and contextual understanding. Medical documentation is often ambiguous, incomplete, or written in ways that require interpretation. AI systems rely on patterns and probabilities, not intent.
For example, AI may struggle with:
Complex or multi-specialty cases
Specialty-specific coding rules
Payer-specific guidelines and local coverage determinations
Modifier usage that depends on clinical judgment
Denials management and appeals
Compliance decision-making during audits
Medical coding is not just about assigning codes. It directly affects reimbursement, compliance, and audit risk. A single incorrect code can lead to claim denials, delayed payments, or even payer recoupments. AI cannot take accountability when these issues arise. Human coders do.
The Role of Certified Medical Coders in an AI-Driven Future
Rather than being replaced, medical coders are becoming more valuable as reviewers, auditors, and compliance experts. As AI handles repetitive tasks, certified coders shift their focus to higher-level responsibilities such as validating AI-generated codes, resolving complex cases, and ensuring payer compliance.
This evolution improves overall accuracy and protects practice revenue. Human oversight is especially critical for practices dealing with Medicare, Medicaid, and commercial payers with strict coding and documentation requirements.
The future of medical coding is not AI versus humans. It is AI plus human expertise.
What This Means for Medical Practices and Billing Companies
Practices that rely solely on AI-based medical coding software risk increased denial rates and compliance issues. Automated systems may miss nuances that experienced coders would immediately recognize.
On the other hand, practices that combine AI-assisted coding with expert medical billing and coding professionals benefit from improved efficiency without sacrificing accuracy. This hybrid approach leads to better claim acceptance rates, reduced rework, and stronger audit readiness.
For medical billing companies, the focus is shifting toward intelligent workflow design, where technology supports coders rather than replaces them.
Final Thoughts: Will AI Replace Medical Coders?
AI will not replace medical coders, but it will replace outdated and inefficient coding workflows. The demand for skilled medical coders who understand compliance, payer rules, and revenue optimization is not decreasing—it is evolving.
The most successful healthcare practices are those that embrace technology while continuing to rely on human expertise to safeguard revenue and compliance.
AI is a powerful tool. Medical coders remain the decision-makers.